Endometriosis: Navigating Pelvic and Menstrual Pain By Lisa De Jong
$5.00
Endometriosis: Navigating Pelvic and Menstrual Pain By Lisa De Jong – Digital Download!
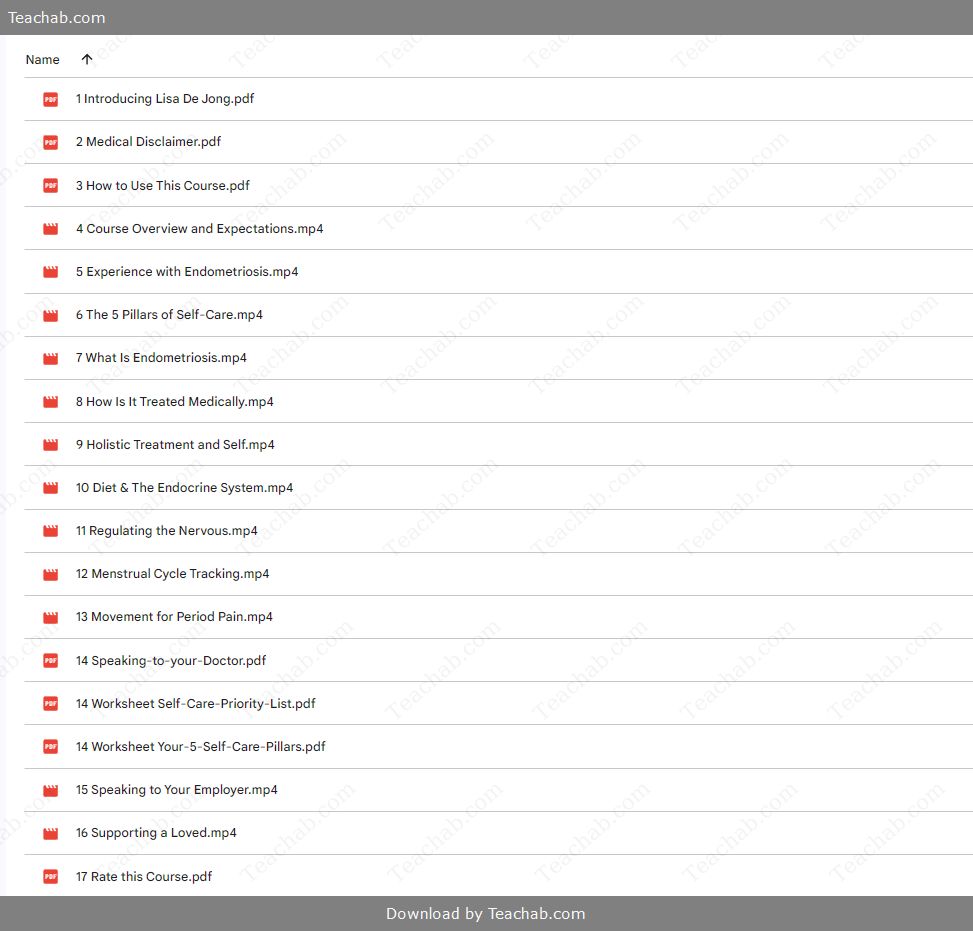
Content Proof:
Endometriosis: Navigating Pelvic and Menstrual Pain by Lisa De Jong
Navigating the turbulent waters of endometriosis can be excruciating both physically and emotionally for those affected. With a prevalence that impacts an estimated 1 in 10 women globally, this chronic condition is characterized by the growth of endometrial-like tissue outside the uterus, leading to debilitating pelvic pain and a myriad of other symptoms. As awareness grows, so does the necessity of understanding how to navigate this complex landscape. This guide offers a comprehensive exploration of endometriosis: from its various forms and symptoms to the diagnostic methods and treatment options available, along with insights into the profound impact it has on the quality of life for those who endure it. Moreover, we will emphasize the importance of community support and advocacy initiatives that can empower individuals on their path to managing this condition. With knowledge as our ally, we can shine a light on the shadows cast by endometriosis, enhancing the journey toward wellness and quality living.
Understanding Endometriosis
Endometriosis is not merely a gynecological condition; it is a complex and multifaceted disorder affecting women on various levels. To draw a parallel, think of it as an unwelcome guest that disrupts the harmony of a home one who plants roots in the living room, kitchen, and beyond, where they wreak havoc. When endometrial-like tissue grows outside the uterus, typically in the pelvis surrounding organs such as the ovaries or the fallopian tubes, it does not behave as it would if it were confined to the uterine cavity. Instead, it thickens and bleeds in response to hormonal changes, triggering an inflammatory response that can lead to chronic pain, dysfunctional menstruation, and even infertility.
Existing research highlights a significant link between endometriosis and mental health, as the constant cycle of pain and the struggle to conceive can lead to frustration, anxiety, and depression. This emotional toll is often exacerbated by the lack of understanding and visibility surrounding the condition, which can leave individuals feeling isolated in their suffering. The metaphorical “unwelcome guest” becomes a constant presence, leading to a sense of entrapment.
Underpinning the understanding of endometriosis are its various manifestations, ranging from the mild discomfort of mild endometriosis to the severe pain resulting from deep infiltrating disease. The type of endometrial tissue growth and the location of these growths significantly influence the symptoms and treatment approaches necessary. Knowledge of these aspects can empower individuals to address their unique experiences with this chronic illness.
To summarize, understanding endometriosis requires recognizing its complexity an unwanted cycle shaped by hormonal influences, pain responses, and a myriad of symptoms that vary widely between individuals. The following sections will delve deeper into the tissue growth types associated with endometriosis, shedding light on the specific characteristics that define this condition.
Types of Endometrial Tissue Growth
The complexity of endometriosis begins with the varying types of endometrial tissue growth that characterizes the condition. Think of this as a diverse landscape where different types of plants might grow in different plots of land each requiring unique care and understanding. The types of endometrial tissue growth include:
- Ectopic Endometrial Glands and Stroma: The most common form of endometriosis, these structures mirror the endometrial lining found inside the uterus but grow outside of it. They are frequently located on the ovaries, fallopian tubes, and peritoneum, leading to inflammation and pain.
- Endometriomas: Often referred to as “chocolate cysts,” these are fluid-filled cysts that develop in the ovaries as a result of endometrial tissue shedding within the cysts. Their thick, dark fluid is akin to the richness of chocolate, but the pain they introduce is far from sweet.
- Peritoneal Endometriosis: This involves the presence of endometrial-like cells on the peritoneum, which lines the abdominal cavity. It is the most prevalent type of endometriosis and often leads to significant inflammation and scarring.
- Deep Infiltrating Endometriosis (DIE): The most severe form of endometriosis, DIE penetrates deeply into pelvic organs, often affecting the bladder, rectum, or ligaments supporting the uterus. This type can lead to debilitating pain and complicated surgical management options.
- Catamenial Pneumothorax: Although rare, this unique manifestation occurs when endometrial tissue is found in the pleural cavity, potentially leading to cyclical respiratory issues correlated with menstrual cycles. It exemplifies how endometriosis can manifest unexpectedly, complicating the overall understanding of the disease.
Understanding these types of endometrial tissue growth opens the door to better diagnostic practices and effective treatment strategies. Working closely with healthcare providers becomes crucial as they navigate the nuances of each case a roadmap that can help minimize pain and enable individuals to reclaim their lives.
Symptoms Associated with Endometriosis
The symptoms of endometriosis often paint a challenging portrait of the daily struggles faced by those affected. Picture a roller coaster: the highs and lows can come suddenly and unexpectedly, leaving individuals feeling unmoored and vulnerable. Common symptoms associated with endometriosis include:
- Pelvic Pain: Perhaps the most prevalent symptom, chronic pelvic pain can be felt before and during menstruation and can vary from infrequent discomfort to debilitating pain that affects everyday life.
- Dysmenorrhea: Women with endometriosis frequently experience severe menstrual cramps, which worsen over time. The pain associated with dysmenorrhea can begin days prior to menstruation, often leaving women unable to partake in their usual activities.
- Pain During Intercourse: This can have profound implications for intimate relationships, as pain during or after sexual activity is commonly reported by those suffering from endometriosis. This symptom can lead to emotional distress and complications within partnerships.
- Fatigue: Chronic fatigue is a frequent complaint among individuals with endometriosis, often exacerbated by the ongoing pain and systemic stressors associated with the condition.
- Gastrointestinal Troubles: Symptoms such as childbirth-like bloating, nausea, diarrhea, constipation, and painful bowel movements can occur, particularly during menstrual periods, further complicating overall well-being.
- Infertility: Endometriosis is a leading cause of infertility in women. The growth of endometrial-like tissue can disrupt normal reproductive function, making it challenging for those who aspire to conceive.
- Other Symptoms: Heavy menstrual bleeding or bleeding between periods may also occur. Depression and anxiety can become prevalent co-morbid conditions due to the chronic nature of the pain and difficulties faced in daily life.
With an estimated 70% of women suffering from chronic pelvic pain related to endometriosis, recognizing these symptoms is crucial for effective management. The emotional turmoil that often accompanies physical symptoms can only compound the experience, highlighting the necessity for comprehensive care strategies that address both physical and mental health needs.
Differentiating Endometriosis From Other Conditions
The diagnostic journey for endometriosis can feel like traversing a winding path; multiple conditions can share symptoms with its narrative, often leading to misdiagnosis. To illustrate this complexity, consider a game of “Guess Who?” where various ailments can masquerade as the enigmatic figure of endometriosis. The following distinctions can help differentiate endometriosis from similar conditions:
- Ovarian Cysts: While both can cause pain, ovarian cysts may resolve independently, whereas endometriosis often manifests with persistent, escalating pain as the condition progresses.
- Fibromyalgia: This condition presents as widespread musculoskeletal pain, which can mimic the chronic pain of endometriosis. Unlike endometriosis, fibromyalgia typically involves generalized body pain rather than localized pelvic discomfort.
- Interstitial Cystitis: Characterized by severe bladder pain and urgency, this condition may overlap with endometriosis symptoms but is primarily attributed to bladder inflammation rather than reproductive system disturbances.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease or ulcerative colitis can present with gastrointestinal symptoms similar to those of endometriosis. However, IBD is intrinsically linked to the gastrointestinal tract, while endometriosis is directly related to the reproductive system.
- Pelvic Inflammatory Disease (PID): This infection-related condition often presents with acute pelvic pain and can be ruled out through signs of infection or other revealing medical history.
Due to the symptom overlap, women often encounter a long and arduous quest for an accurate diagnosis, typically taking between 7 and 12 years from the onset of symptoms. The understanding of these distinctions is essential for empowering women to seek the right medical interventions and ultimately improve their quality of life.
Diagnosis of Endometriosis
The journey toward an accurate diagnosis of endometriosis often begins with a detailed assessment of a patient’s medical history and symptoms. To liken it to a detective story, healthcare providers must gather clues that provide insight into the underlying condition:
- Symptom Review and Medical History: A thorough assessment includes details about pelvic pain, heavy menstrual bleeding, and any challenges related to fertility. The patient’s medical background, family history, and menstruation patterns are equally important to establish a comprehensive picture.
- Pelvic Examination: During a pelvic exam, providers physically palpate the pelvic region to identify any abnormalities such as cysts or scarring, which can indicate the presence of endometriosis.
- Imaging Studies: While imaging cannot definitively diagnose endometriosis, they can help visualize cysts or lesions associated. Common imaging tests include:
- Ultrasound: Often the first line of investigation, transvaginal ultrasound can highlight ovarian endometriomas.
- Magnetic Resonance Imaging (MRI): For more detailed evaluation, MRI provides a comprehensive view of the pelvic region and can aid in mapping extensive cases of endometriosis.
- Laparoscopy: The gold standard for diagnosing endometriosis, this minimally invasive surgical procedure allows for direct visualization of pelvic organs. If endometrial-like tissues are found, biopsy samples can be taken for histological confirmation.
- Biopsy: The definitive confirmation of endometriosis is often achieved through a biopsy during laparoscopy, in which tissue specimens are analyzed for the presence of endometrial-like cells.
Navigating the diagnostic process can be fraught with challenges, underscoring the importance of awareness regarding the complexity of endometriosis.
Clinical Diagnosis Procedures
Clinically diagnosing endometriosis involves a multifaceted approach that combines patient history, physical examinations, imaging techniques, and surgical intervention. This process is akin to piecing together a jigsaw puzzle where each piece sheds light on the broader picture of endometriosis.
- Initial Assessment: The first step in diagnosis involves collecting detailed symptoms and medical histories from patients. This information serves as the foundation for further evaluation, fostering a connection between the healthcare provider and the patient.
- Physical Examination: A thorough pelvic examination allows healthcare providers to feel for any physical abnormalities, including tender areas or disparate masses that might be produced through endometrial growth.
- Imaging Techniques: High-definition imaging techniques like ultrosound and MRI play an essential role in visualizing potential cysts or lesions associated with endometriosis, thus narrowing down diagnosis.
- Laparoscopy: While imaging can hint at the presence of endometriosis, laparoscopy remains the definitive method for diagnosis. This surgical procedure allows providers to inspect the pelvic cavity and assess the extent of the disease. The healthcare team can excise lesions or take biopsies for further examination, which is critical for confirming endometriosis.
- Post-Procedure Follow-up: After surgical intervention, comprehensive follow-up care assists in managing symptoms and monitoring the patient’s recovery while providing additional education on ongoing treatment options.
Understanding the clinical diagnosis procedures lends insight into the comprehensive pathway required for accurate identification and effective treatment, emphasizing the importance of thorough and individualized care.
Role of Imaging Techniques
Imaging techniques serve as invaluable tools in diagnosing endometriosis, where each modality unveils layers of information about this complex condition. Think of imaging as the flashlight illuminating potential hidden corners of diagnostics.
- Transvaginal Ultrasound (TVUS): This method is increasingly employed in the diagnosis of endometriosis, particularly for visualizing ovarian endometriomas. It is a non-invasive procedure providing immediate insights into the presence of cysts, guiding decisions for further intervention.
- Magnetic Resonance Imaging (MRI): MRI technology provides exhaustive detail about pelvic structures and is particularly useful for visualizing deep infiltrating endometriosis. The high-contrast images allow healthcare providers to delineate the extent of the disease and plan pre-surgical approaches.
- Limitations of Imaging: While imaging techniques enhance diagnostic accuracy, they have limitations. For example, some forms of endometriosis may not present on imaging until more severe stages of the disease, necessitating the combination of imaging with other diagnostic approaches like laparoscopy.
- Biopsy and Laparoscopy: Ultimately, imaging techniques facilitate the identification of endometrial-like tissue but do not replace the need for definitive procedures. Biopsy performed during laparoscopic surgery guarantees a solid diagnosis, analyzing histological samples for confirmation.
In summary, imaging plays a pivotal role in diagnosing endometriosis its integration into clinical practice is essential in streamlining patient care within diagnostic odysseys, leading to more timely and accurate interventions.
Importance of Biopsy and Laparoscopy
In the journey of diagnosing endometriosis, laparoscopy and biopsy emerge as critical components of confirming the presence of endometrial-like tissue growth outside the uterus, akin to the final pieces of a puzzle that reveal the complete picture.
- Laparoscopy Explained: Laparoscopy is considered the gold standard for the diagnosis of endometriosis. Through small incisions, the surgeon utilizes a laparoscope a slender tube equipped with a camera to visualize the abdominal cavity. This viewing allows for direct assessment of the organs for any misplaced endometrial-like tissue.
- Diagnostic Accuracy: The accuracy of laparoscopy in establishing a diagnosis for endometriosis cannot be overstated. It allows for immediate assessment of the extent of the disease, and its minimally invasive nature reduces the patient’s recovery time compared to full laparotomy.
- Biopsy Significance: During laparoscopic procedures, tissue samples can be collected for histological examination. This biopsy is crucial as it confirms the diagnosis by identifying specific endometrial-like cells. This histological confirmation is vital for determining treatment options and evaluating disease severity.
- Disease Management Post-Diagnosis: Identifying the type and extent of endometriosis through laparoscopy informs patient-centered treatment decisions, as a clear diagnosis is integral to shaping individualized management plans.
- Psychological Impact: The knowledge gained from a definitive diagnosis can alleviate some uncertainty and fear, empowering individuals to actively participate in their treatment journey.
In essence, biopsy and laparoscopy not only affirm the diagnosis of endometriosis but also constitute a pathway toward targeted management strategies that incorporate the unique characteristics of each patient’s experience with the disease.
Treatment Options for Endometriosis
When faced with the multitude of symptoms and challenges posed by endometriosis, treatment options vary significantly based on individual needs, pain levels, and goals such as fertility. This array of approaches can be visualized as different roads leading to potential relief, each with its unique obstacles and landmarks.
- Hormonal Treatments: These are often the frontline treatment options aimed at regulating hormonal levels to reduce endometrial growth. Options include:
- Progestins: Hormonal birth control methods containing progestin are frequently utilized to alleviate symptoms and regulate menstrual cycles.
- Combined Oral Contraceptives: These pills can help minimize heavy periods and reduce painful symptoms associated with the cycle.
- GnRH Agonists: Acts by suppressing estrogen production, inducing a temporary menopause-like state that can help shrink endometrial lesions.
- Non-Hormonal Treatments: While hormonal therapies are popular, non-hormonal options are also useful in managing pain:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Commonly prescribed to alleviate pain and cramping, NSAIDs can be part of a comprehensive pain management strategy.
- Pain Management Strategies: This category encompasses lifestyle changes, physical therapy, acupuncture, and alternative therapies aimed at overall well-being.
- Surgical Interventions: When conservative approaches fail to provide relief, surgical options may be explored:
- Laparoscopic Surgery: Effective in removing endometriotic lesions, laparoscopic surgery can alleviate pain and improve fertility.
- Hysterectomy: In cases of severe, treatment-resistant endometriosis especially for women not seeking to conceive hysterectomy (with or without oophorectomy) can be a last-resort option.
- Integrative Approaches: Including mindful practices, nutritional changes, or herbal treatments can enhance quality of life. Some studies suggest that dietary interventions, supplements, and complementary therapies can mitigate symptoms for particular individuals.
- Patient-Centered Care: Tailoring treatment options to meet individual needs is essential. Women living with endometriosis benefit from open dialogue with healthcare providers, refining portfolios of treatments via feedback on efficacy and tolerance.
Providing the right combination of treatments can mean the difference between debilitating pain and manageable symptoms, emphasizing the critical role of individualized care in successfully navigating endometriosis.
Medical Management Approaches
Medical management of endometriosis largely revolves around hormonal therapy, pain management, and lifestyle modifications. Together, these elements form a comprehensive arsenal against the disorder.
- Hormonal Intervention: As established in earlier sections, hormonal therapies, especially progestins and oral contraceptives, play a pivotal role in minimizing the effects of estrogen, which stimulates endometrial growth. The goal is to reduce or eliminate menstruation in some cases, effectively managing symptoms and preventing disease progression.
- Pain Management: Chronic pain often requires specialized approaches beyond typical analgesics, leading to strategies that may include:
- NSAIDs: As a go-to option, they alleviate pain while reducing inflammation a common component of endometriosis.
- Neuropathic Pain Medications: Drugs like gabapentin can be beneficial in cases where traditional pain treatments are inadequate, addressing the nerve-related pain associated with chronic conditions.
- Lifestyle Modifications: Small, workable changes in lifestyle can produce big results. Regular exercise, balanced diets rich in omega-3 fatty acids, and managing stress through mindfulness or yoga can significantly enhance quality of life and symptom management.
- Role of Physical Therapy: Incorporating physical therapy, especially pelvic floor therapy, has shown beneficial outcomes in managing pelvic pain. This specialized approach can help individuals relax tense muscles and enhance well-being.
- Mental Health Consideration: Given the emotional toll associated with endometriosis, integrating mental health support into treatment plans is vital. Therapy, support groups, and other mental health resources facilitate coping mechanisms and enhance resilience.
Emphasis on a holistic, patient-centered approach allows for flexibility in medical management, ensuring tailored solutions to meet the diverse and unique challenges posed by endometriosis.
Surgical Interventions and Their Efficacy
When medical management strategies do not sufficiently alleviate symptoms of endometriosis, surgical interventions become a vital consideration. Picture surgery as a sculptor delicately carving away excess materials from a stone, revealing a smoother, more manageable surface. The efficacy of surgical interventions varies based on the type and extent of endometriosis:
- Laparoscopic Surgery: This minimally invasive option allows surgeons to visualize and remove endometrial-like tissue through small incisions. Research indicates that patients experience significant pain relief and improvements in quality of life following laparoscopic procedures.
- Laparotomy: For more extensive cases of endometriosis, a laparotomy (a larger abdominal incision) may be warranted. While this method allows for comprehensive exploration and excision of tissue, it carries longer recovery times and more significant surgical risks.
- Ablation Techniques: Some surgeries focus on ablation destroying endometrial lesions through thermal methods. These procedures are generally suited for patients with mild to moderate endometriosis but do not involve complete tissue removal, which may leave a risk of recurrence.
- Hysterectomy: Considered a last-ditch effort for those no longer wishing to conceive, a hysterectomy can significantly reduce symptoms for some women by eliminating the reproductive organs. However, this procedure leads to irreversible infertility and is typically accompanied by hormone replacement therapy post-operation to address sudden hormonal changes.
- Rehabilitation and Follow-up: Post-surgery, individuals might need support via rehabilitation services, including pelvic floor therapy, to facilitate a smooth recovery while maximizing the therapeutic effects of surgery.
In conclusion, understanding the significance and potential of surgical interventions in treating endometriosis serves as a beacon for those facing debilitating pain and seeking effective long-term solutions.
Integrative and Complementary Therapies
Integrative and complementary therapies offer promising adjuncts to traditional medical and surgical treatments for endometriosis. When taken together, these approaches can cultivate improved overall health and wellness akin to tending a varied garden where different plants flourish side by side.
- Acupuncture: Supported by emerging evidence, acupuncture has been recognized as a potentially beneficial treatment for endometriosis-related pain. Involving the insertion of thin needles into specific body points, acupuncture aims to enhance energy flow and alleviate pain effectively acting as a calming distraction from symptoms.
- Nutritional Interventions: Evidence suggests that adopting a whole-food diet rich in anti-inflammatory properties can help manage endometriosis symptoms. This includes increasing the intake of omega-3 fatty acids, fresh vegetables, and avoiding trans fats, caffeine, and refined sugars.
- Physical Therapy: Specialized pelvic floor physical therapy focuses on relieving pain rooted in muscle tightness and dysfunction. By incorporating targeted exercises, breath work, and muscle relaxation techniques, individuals can experience significant pain relief and greater comfort in daily activities.
- Herbal Remedies: While some women report success with herbal treatments, the scientific backing remains limited, warranting caution. Seeking guidance from a qualified practitioner can help ensure safe and effective use.
- Mind-Body Therapies: Techniques such as yoga, meditation, and mindfulness can improve emotional resilience and coping mechanisms while simultaneously addressing physical tension often accompanied by chronic pain. Not only do these practices foster relaxation, but they can also enhance overall well-being.
Ultimately, integrative and complementary therapies reveal that treating endometriosis doesn’t have to rely solely on conventional medicine. Utilizing a multifaceted approach enables women to construct personalized treatment plans that resonate with their lifestyles and individual needs.
Management of Pelvic Pain
Pelvic pain management requires a holistic understanding of chronic versus acute pain, especially when it intersects with conditions like endometriosis. Picture chronic pelvic pain (CPP) as a relentless storm affecting daily life in varied ways while acute pelvic pain is more akin to a sudden lightning strike, causing immediate concern.
Chronic vs. Acute Pelvic Pain
Chronic pelvic pain (CPP) refers to discomfort lasting longer than six months, often associated with endometriosis, and significantly affects quality of life. With around 15% of women experiencing CPP, the nuances of complex conditions must be taken into account.
- Persistent vs. Sudden Pain: Unlike acute pain, which can arise quickly from conditions like appendicitis or ectopic pregnancy, chronic pain is often deeply rooted, requiring ongoing evaluation and management strategies that address both symptom relief and underlying causes.
- Management Strategies for CPP: Managing chronic pelvic pain typically necessitates a multidisciplinary approach as it may involve multiple aspects of care, including medication management, physical therapy, psychological support, or surgical interventions when necessary.
- Emotional and Psychological Health: The interconnection of chronic pelvic pain with psychological health cannot be overlooked. Many individuals experiencing CPP also grapple with anxiety and depression, highlighting the importance of comprehensive support.
- Patient-Centered Care: Through tailored management strategies, including various pain-relief modalities, health providers can offer targeted care that aligns with the patient’s experiences and preferences.
- Referral to Specialists: Given the complexity of CPP, individuals often benefit from referrals to specialists such as gynecologists, pain management experts, and pelvic floor physical therapists.
In contrast, acute pelvic pain often demands swift diagnostic focus, as the potential for serious medical complications necessitates immediate attention.
Pain Management Strategies
Pain management strategies are critical in navigating the challenges posed by endometriosis, affording symptomatic relief while restoring overall function. This multifaceted approach can be likened to assembling a toolkit comprising various tools, each serving a distinct purpose.
- Comprehensive Assessment: Beginning with a thorough assessment of symptoms and individual pain responses, healthcare providers can work collaboratively to design tailored approaches that suit each unique situation.
- Medications: Pharmacologic interventions may include:
- NSAIDs: These are often a first-line treatment, providing relief from inflammation and pain associated with menstruation.
- Hormonal Therapies: Employed to manage pain and regulate hormonal fluctuations.
- Neuropathic Agents: Medications like gabapentin may be utilized for pain stemming from nerve-related complications.
- Physical Therapies: Engaging in targeted physical therapy, including pelvic floor rehabilitation, can diminish muscle tension, improve coordination, and promote pelvic health.
- Behavioral Interventions: Cognitive-behavioral therapy (CBT) and mindfulness practices bolster emotional management, equipping individuals with coping strategies for handling chronic stress associated with pain.
- Surgical Options: In severe cases where medications and physical therapies do not yield satisfactory results, surgical interventions to remove endometrial lesions may become essential for long-term improvement.
Implementing a comprehensive suite of pain management strategies can help individuals reclaim their quality of life, facilitating a proactive role in navigating the complexities of endometriosis.
Patient-Centered Care Plans
When devising effective treatment pathways for endometriosis, consultant strategies adopt a patient-centered approach this mirrors the idea of individualizing a garden to meet diverse plant needs. Patient-centered care fosters communication and empathy, allowing individuals to feel heard and supported throughout their treatment.
- Comprehensive Patient Assessment: Establishing a complete baseline assessment is crucial, wherein providers gather detailed histories, active symptoms, and treatment preferences to inform their strategies.
- Collaborative Goal Setting: Engaging in shared decision-making with patients allows healthcare providers to set realistic goals for intervention, fostering a sense of ownership and commitment to the treatment plan.
- Utilization of Multi-Disciplinary Teams: Integrating a multi-disciplinary approach incorporates gynecologists, pain management specialists, nutritionists, and mental health experts to address the holistic needs of patients.
- Continuous Monitoring and Adjustments: Regular follow-ups ensure that treatment plans remain relevant and adaptive to changing patient needs. Collecting feedback on medication efficacy or symptom prevalence enhances the decision-making process.
- Emphasis on Education and Advocacy: Empowering individuals through education about their condition, treatment options, and self-advocacy fosters greater confidence in managing their health.
The focus on patient-centered care plans ensures that treatment aligns effectively with individual identities and experiences, steering away from a one-size-fits-all paradigm to facilitate enhanced outcomes for those battling endometriosis.
Impact of Endometriosis on Quality of Life
The repercussions of endometriosis extend beyond the physical realm and into the very fabric of a woman’s quality of life. Just as ripples radiate across a still pond, the effects of chronic pain resonate throughout various aspects, intertwining with emotional well-being and social connections.
Psychological Effects and Emotional Well-Being
Endometriosis often inflicts profound psychological effects on individuals, contributing to a cycle of emotional turmoil. It is akin to carrying a load that grows heavier with every step taken leading to frustration, grief, and often despair.
- Mental Health Challenges: Research indicates that women with endometriosis experience higher rates of depression, anxiety, and stress-related disorders, largely stemming from the relentless nature of chronic pain and fertility challenges.
- Social Isolation: The unpredictable nature of endometriosis symptoms can lead to social withdrawal. Many individuals may cancel plans or shy away from social events to avoid potential discomfort or embarrassment, contributing to heightened feelings of loneliness.
- Impact on Relationships: The interplay between endometriosis and intimacy often complicates personal relationships. Pain during sexual intercourse can introduce strain, leading to emotional distance between partners as they grapple with understanding the condition and its effects on intimacy.
- Coping Mechanisms: Building resilience through support networks, therapy, and open communication can aid in managing psychological challenges. Sharing experiences with others who understand the struggle can provide vital relief.
- Awareness and Support: Raising awareness about the psychological implications of endometriosis fosters a greater understanding of the condition among friends and family, paving the way for nuanced support and compassion.
In navigating the intertwined relationship between endometriosis and mental health, understanding and bolstering emotional well-being is paramount.
Social and Relationship Challenges
Beyond individual emotional challenges, the social and relational impacts of endometriosis create a cascade of challenges that can complicate daily functioning.
- Romantic Relationships: The discomfort, unpredictability, and pain associated with endometriosis can contribute to stress within romantic partnerships. A significant percentage of women report that their condition has negatively affected their sexual relationship, leading to feelings of inadequacy or frustration.
- Friendships and Social Connections: The necessity to prioritize health often results in missed gatherings or the need to adjust social activities. Such changes can strain friendships and reduce the sense of community, leading to feelings of isolation.
- Family Dynamics: Family relationships can also be impacted, as partners, parents, or children may struggle to understand the implications of the chronic condition. This lack of understanding may result in communication breakdowns or emotional tension, heightening stress for the patient.
- Work-Life Imbalance: Poorly managed symptoms of endometriosis can hinder consistent work attendance and productivity. As a consequence, individuals may grapple with job-related stress, creating further layers of anxiety and depressive symptoms.
- Building Support Systems: Encouraging familial support and open communication about endometriosis can create healthier dynamics and promote collective understanding, allowing for smoother navigation through relational challenges.
Addressing the impact of endometriosis on social relationships requires enhanced communication both within personal connections and efforts to foster broader societal understanding of the impact of this condition.
Work and Daily Life Considerations
Living with endometriosis can create unique challenges within the workplace and daily life, necessitating strategic consideration to cope effectively. Each individual’s experience may vary, but certain commonalities emerge in navigating these challenges.
- Workplace Accommodations: Many women face difficulties maintaining consistent work attendance, leading to challenges related to performance evaluations and job security. Flexible work schedules, accessible healthcare resources, or supportive workplace policies become essential for managing endometriosis symptoms.
- Disclosures and Communication: Deciding whether to disclose a chronic condition to employers remains a significant consideration. Open communication about flexible working options and impacts on productivity can foster a more supportive work environment.
- Job Stress: The pressures of managing endometriosis symptoms alongside career responsibilities can contribute to excessive stress, potentially leading to burnout. Establishing clear boundaries and setting realistic expectations can aid in managing this duality of stressors.
- Impact on Daily Activities: Chronic pain can affect day-to-day responsibilities including care for children, household duties, and personal activities exacerbating feelings of helplessness. Time management strategies and seeking assistance when needed can help alleviate these burdens.
- Supportive Resources: Referrals to occupational health services, employee assistance programs, or counseling services may facilitate coping strategies tailored to the individual’s needs, improving overall daily functioning.
In recognizing and addressing the complexities that endometriosis introduces into work and daily life, individuals can confront these challenges with tailored strategies that help create a more manageable existence.
Research and Current Trends in Endometriosis
The landscape of endometriosis research has evolved rapidly in recent years, necessitating a close look at emerging trends, innovative treatments, and advancing scientific understanding of the condition.
Advances in Medical Research
The past few years have seen considerable investment in endometriosis research, driven by a collective drive for improved diagnosis, treatment, and quality of life for those affected.
- Funding and Awareness Initiatives: As public awareness grows, governmental bodies, non-profits, and advocacy groups are stepping up to secure funding for essential research demonstrating a commitment to individuals grappling with endometriosis.
- Focus on Disease Mechanisms: Research efforts have increasingly zeroed in on the mechanisms behind endometriosis’ development. Understanding hormonal fluctuations, inflammatory responses, and the role of genetics is pivotal for creating targeted therapies.
- Diagnostic Innovations: Recognizing the challenges within diagnostic pathways, new clinical guidelines emphasize integrating innovative imaging techniques, which may help decrease the time from symptom onset to diagnosis.
- Disease Mapping: New imaging technologies combined with artificial intelligence and machine learning are paving the way for precise mapping of endometrial tissue and deeper insights into disease severity.
- Patient Engagement in Research: Engaging individuals living with endometriosis in the research process fosters a deeper understanding of their unique needs, leading to more relevant therapeutic developments.
This momentum reflects an evolving commitment to unraveling the complexities surrounding endometriosis, ultimately aiming to enhance care and treatment outcomes.
Innovations in Treatment Modalities
Innovations in the treatment landscape for endometriosis have led to diversification in therapeutic options available to patients, promising new avenues of relief and engagement.
- Emerging Treatment Strategies: Novel treatment modalities are being explored, including photodynamic therapy, gene therapy, and immunotherapy. These lines of inquiry seek to customize therapies according to individual patient needs, offering further advancements in symptom management.
- Hydrogel Implants: Research has unveiled promising hydrogel implants intended for the fallopian tubes, potentially preventing retrograde menstruation a mechanism believed to underpin the development of endometriosis.
- Precision Medicine Approaches: The shift towards precision health signifies an evolution in treatment paradigms, encouraging the exploration of patient-specific factors (like genetics and microbiome) to optimize therapeutic responses.
- Holistic Support Strategies: Continued emphasis on integrative methods such as dietary modifications and complementary therapies has encouraged further acceptance of multi-faceted approaches in endometriosis management.
- Clinical Trials and Investigations: Ongoing clinical trials exploring new medications and treatment strategies signify an active commitment to finding effective solutions that resonate with current patient needs and experiences.
These contingent forces harmonize to shift the perceptions and practices surrounding endometriosis care, ultimately paving the way for improved outcomes.
Future Directions in Endometriosis Care
Future directions in endometriosis care point toward a more inclusive, personalized approach to treatment, centering on the unique experiences and diverse needs of patients.
- Holistic Approaches: As understanding increases surrounding the multifaceted nature of endometriosis, the focus will likely shift toward comprehensive models incorporating physical, emotional, and social dimensions of care.
- Patient Involvement: Involving patients throughout the care continuum will promote shared decision-making and patient advocacy, ensuring their experiences and preferences take precedence in therapeutic discussions.
- Collaborative Research Efforts: Partnerships between researchers, healthcare providers, and influential organizations will explore innovative solutions, addressing gaps in knowledge and experience, leading to enhanced research outcomes.
- Increased Advocacy and Policy Focus: The heightened visibility around endometriosis engenders actions toward reform in healthcare policies and increased access to vital resources for those affected.
- Long-term Monitoring and Outcomes: Future iterations of care will be informed by long-term perspectives, ensuring that successful outcomes equate to sustained improvements in quality of life for individuals with endometriosis.
Ultimately, the trajectory of endometriosis care is poised for transformation as researchers, advocates, and patients collaborate to reshape the narrative around this chronic condition, advocating for improved care and understanding.
Patient Advocacy and Support Resources
Awareness and advocacy play an integral role in improving the lives of those living with endometriosis. Just as community villages come together to support one another, so too can patient advocacy efforts create a robust support network for individuals facing the condition.
Importance of Community Support Groups
Strong community support groups foster understanding and camaraderie, creating spaces where individuals can share their experiences and resources.
- The Role of Advocacy Organizations: Advocacy groups, like the Endometriosis Foundation of America, work tirelessly to secure funding and raise awareness. Initiatives such as the Endometriosis CARE Act showcase how collective efforts can bring about legislative changes that support endometriosis research.
- Emotional Support Networks: Community-based support groups facilitate connections among individuals dealing with similar challenges. These safe havens allow women to voice their concerns, creating validation and a platform for sharing coping strategies.
- Educational Resources: Informed support networks can provide valuable educational resources for individuals looking to better understand their condition, available treatments, and self-care practices.
- Peer Mentorship: Connections forged within support groups can inspire peer mentorship opportunities, enabling individuals to provide guidance and encouragement to others navigating the challenges associated with endometriosis.
- Promoting Awareness Initiatives: Increased networking fosters the sharing of awareness initiatives. Being involved in community outreach programs can provide individuals a significant conduit to help disseminate essential information about endometriosis, reducing stigma and enhancing understanding.
The power of community support groups can wield significant influence in raising awareness and providing comfort to those engaged in their own struggles with endometriosis.
Educational Resources for Patients
Providing ample educational resources is critical for cultivating informed individuals who can navigate endometriosis with confidence. Empowerment through knowledge is akin to having a reliable compass guiding one’s journey.
- Endometriosis Foundation of America: Founded to raise awareness and provide education, EndoFound offers new insights into the condition, including symptom guides, management strategies, and links to local resources.
- Society for Women’s Health Research: Their endometriosis advocacy toolkit equips patients with information to engage with legislators, raise awareness, and promote financial support for research efforts.
- Clinical Guidelines: Update clinical guidelines provide patients with evidence-based recommendations around symptom management and treatment options, enhancing their understanding of the condition.
- Online Platforms and Forums: Virtual platforms create a space for diverse voices to share their stories, learn from one another, and connect with advocates and healthcare providers specializing in endometriosis.
- Workshops and Educational Seminars: Local and online events designed to educate patients about endometriosis, management options, and coping strategies strengthen awareness and empower communities.
Collectively, these educational resources cultivate informed engagement with endometriosis and foster more nuanced interactions with healthcare providers.
Navigating the Healthcare System for Optimal Care
Navigating the complexities of the healthcare system can often feel overwhelming, particularly for individuals experiencing chronic conditions like endometriosis. However, equipping oneself with information and resources can ease the process.
- Patient Advocacy Programs: Organizations specializing in endometriosis often offer advocacy programs that facilitate education around rights, health insurance, and access to care.
- Comprehensive Care Models: Seeking healthcare providers who practice comprehensive care models allow patients to coordinate their treatment effectively across specialists. This ensures a cohesive approach toward managing endometriosis.
- Community Education Initiatives: Engaging in local community health initiatives can increase awareness of endometriosis, shaping a better understanding of the condition among healthcare providers and the public.
- Developing a Care Plan: Collaboratively developing a personalized care plan with healthcare providers enhances clarity surrounding treatment goals while establishing a pathway for managing symptoms.
- Utilization of Patient Navigators: Utilizing patient navigators can facilitate smoother care coordination and communication among healthcare providers, reducing the burden of navigating the healthcare system alone.
Accessible information, advocacy, and crafted care plans empower individuals to navigate the complexities of the healthcare system successfully, instilling confidence in their healthcare journeys.
In conclusion, the multifaceted nature of endometriosis a chronic condition intricately affiliated with physical, emotional, and social dimensions calls for a comprehensive understanding and careful navigation. By illuminating each aspect of the endometriosis journey from understanding its symptoms to exploring treatment options, fostering community support, and advocating for better care we embrace the power of collective knowledge and solidarity. The path toward enhanced quality of life becomes clearer as individuals confront the challenges posed by endometriosis, bestowing hope and the opportunity to reclaim their narratives in the face of adversity.
Frequently Asked Questions:
Business Model Innovation: We use a group buying approach that enables users to split expenses and get discounted access to well-liked courses.
Despite worries regarding distribution strategies from content creators, this strategy helps people with low incomes.
Legal Aspects to Take into Account: Our operations’ legality entails several intricate considerations.
There are no explicit resale restrictions mentioned at the time of purchase, even though we do not have the course developers’ express consent to redistribute their content.
This uncertainty gives us the chance to offer reasonably priced instructional materials.
Quality Assurance: We guarantee that every course resource you buy is exactly the same as what the authors themselves are offering.
It’s crucial to realize, nevertheless, that we are not authorized suppliers. Therefore, the following are not included in our offerings:
– Live coaching sessions or calls with the course author.
– Entry to groups or portals that are only available to authors.
– Participation in closed forums.
– Straightforward email assistance from the writer or their group.
Our goal is to lower the barrier to education by providing these courses on our own, without the official channels’ premium services. We value your comprehension of our distinct methodology.
Be the first to review “Endometriosis: Navigating Pelvic and Menstrual Pain By Lisa De Jong” Cancel reply
You must be logged in to post a review.

 Kings Initiation - Inception: How to Be a King in a World Of Cowards by Elliott Hulse
Kings Initiation - Inception: How to Be a King in a World Of Cowards by Elliott Hulse 















Reviews
There are no reviews yet.