Destigmatising STIs: Understand Sexually Transmitted Infections By Evelin Dacker
$5.00
Destigmatising STIs: Understand Sexually Transmitted Infections By Evelin Dacker – Digital Download!
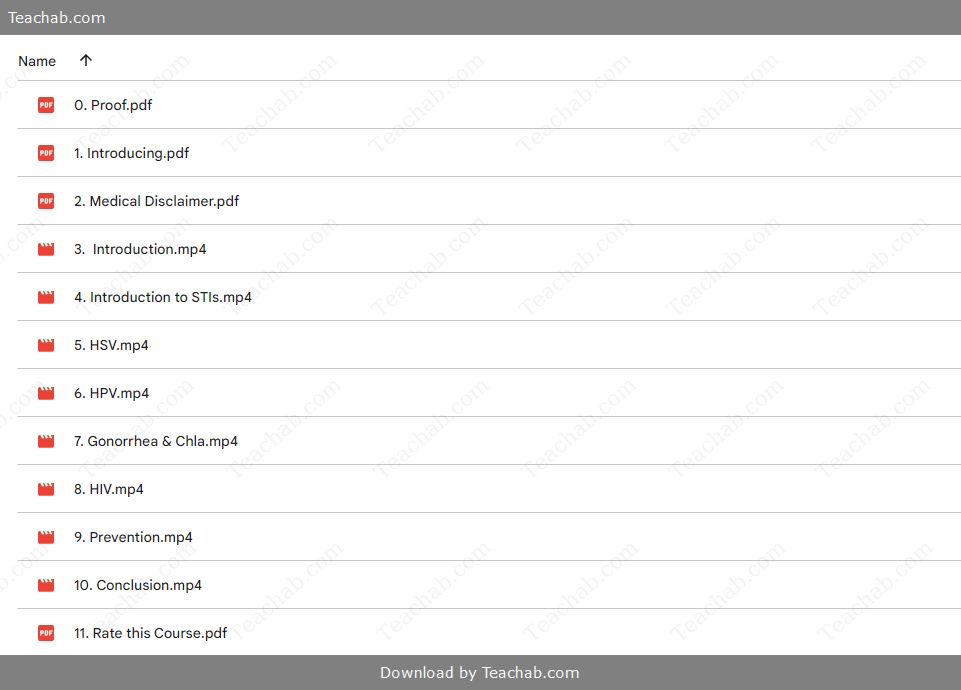
Content Proof:
Destigmatising STIs: Understand Sexually Transmitted Infections by Evelin Dacker
Sexually transmitted infections (STIs) are often shrouded in stigma that profoundly affects public health and individual well-being. This stigma stems from historical misunderstandings, cultural perceptions, and social attitudes towards sexual health that continue to perpetuate shame and discrimination. In contextualizing this stigma, we can explore its roots, dissect social misconceptions, and outline the urgent need for destigmatisation efforts. Dr. Evelin Dacker champions a comprehensive overhaul of how we discuss and understand STIs. Through progressive education and open dialogues, we can foster a healthier society that prioritizes prevention, supportive relationships, and respect for all, regardless of their health status. By understanding the dynamics of STI stigma, we can create pathways for effective intervention and policy change that not only addresses public health concerns but also instills a sense of empowerment among individuals affected by STIs.
Understanding the Stigma Surrounding STIs
Experiencing stigma is akin to living under a cloud that darkens everything; it distorts perceptions, leads to isolation, and fosters a culture of silence. Stigma surrounds STIs primarily due to misconstrued beliefs about how these infections manifest within society. Just as weeds choke the healthy growth of a garden, stigma can stifle open discussions and positive health interactions with individuals regarding STIs, causing them to shy away from seeking necessary medical assistance out of fear of judgement.
Many people harbor misconceptions that STIs arise solely from promiscuity or deviant behavior, leading to a toxic cultural narrative that labels affected individuals as morally inferior. Such simplistic comparisons overshadow the reality that STIs can affect anyone, regardless of their lifestyle choices. A comprehensive understanding of STIs that strips away these misconceptions is ultimately essential for destigmatisation.
Moreover, research supports the argument that stigma operates as a barrier to seeking care, similar to how walls inhibit entry. For instance, individuals often avoid STI testing or treatment due to fears of judgement or shame. This avoidance can perpetuate the very problems these individuals hope to resolve, leading to heightened anxiety, relationship issues, and overall health deterioration. Addressing these perceptions through education and community outreach can cultivate a shift toward a more compassionate understanding, where individuals feel safe to discuss their conditions openly.
To combat the stigma effectively, it is paramount to focus on evidence-based strategies designed to educate the public. Key strategies may include:
- Integrating STI information into sexual health curricula in schools to demystify these infections from a young age.
- Establishing public campaigns focusing on real stories from individuals living with STIs to foster empathy and understanding.
- Encouraging open discussions on social platforms that normalize STI conversations in a non-judgmental way.
In essence, challenging stigma is not just about addressing misinformation; it’s about fundamentally altering societal narratives that shape how we understand and treat individuals living with STIs.
Historical Context of STI Stigma
The history of STI stigma is intrinsically tied to the evolution of societal attitudes towards sex and sexual health. Just as ancient civilizations used to associate illnesses with moral failings, the early years of the HIV epidemic reinforced this damaging narrative. In the 1980s, HIV was disproportionately linked to marginalized communities, especially gay men, further entrenching stigma into discussions of sexual health. This ‘gay disease’ label created an environment of fear, ignorance, and discrimination, resulting in profound psychological ramifications that are still felt today.
As we progressed through the decades, it became evident that the stigma surrounding STIs is not limited to HIV but extends to many infections such as chlamydia, gonorrhea, and syphilis. These infections, viewed through a lens of moral judgement, have created barriers to open conversations. Just as an untreated wound festers, the silence surrounding STIs can lead to the compounding of public health crises, exacerbating rates of transmission and preventing individuals from seeking treatment.
The roots of stigma also intertwine with social inequities related to race, gender, and sexual orientation. Those from marginalized communities bear a disproportionate burden of STI stigma, which can result in inequitable access to health services. Systemic barriers can perpetuate a cycle of mistrust toward the healthcare system, causing individuals to avoid seeking necessary care.
In addressing these historical narratives, it becomes crucial to recognize that stigma is not an inherent characteristic of STIs themselves but rather a social construct that can be dismantled. Transformative strategies include:
- Developing inclusive health policies that actively combat discrimination based on a person’s sexual history.
- Enabling community-based interventions that involve local leaders to reshape conversations about STIs.
- Encouraging educational institutions to provide comprehensive sexual education that includes the historical context of STIs to foster deeper understanding.
By acknowledging the historical context of STI stigma, we can begin to understand the complex interplay of factors contributing to the greater public health landscape and work towards a more informed and empathetic society.
Social Perceptions and Misconceptions
Social perceptions and misconceptions surrounding STIs can significantly influence public attitudes and health behaviors. One common myth is the association of STIs with promiscuity, creating an unjust narrative that stigmatizes affected individuals. This misbelief not only oversimplifies the complex realities of how STIs are spread but also perpetuates shame among those seeking care. This stigma acts as a barrier that inhibits individuals from accessing timely testing and treatment akin to a glass wall that keeps them isolated from the help they need.
In addition to misconceptions about promiscuity, many people mistakenly believe that STIs can only be transmitted through sexual intercourse. For instance, the fear of transmission through everyday contact can lead individuals to avoid necessary discussions about STIs and further isolate those living with these infections. Education serves as a critical antidote to this misunderstanding, highlighting that knowledge is power. Key elements of effective education might include:
- Addressing the factual modes of transmission, including emphasizing that many STIs can be contracted even by those who consider themselves to be in monogamous relationships.
- Utilizing relatable analogies to explain common routes of STI transmission for instance, likening the transmission of STIs through intimate contact to how germs spread through physical contact, dispelling the notion that personal behavior is solely to blame.
Furthermore, the impact of stigma on prevention and treatment goes beyond individual experiences; it extends into community health outcomes. When individuals avoid seeking care due to fears of judgment, it exacerbates the cycle of undetected infections in the community. Studies have found that people in stigmatized groups are less likely to communicate openly about testing and treatment, damaging public health initiatives that aim to lower STI rates.
As we seek to dismantle these damaging perceptions, we must also take proactive steps to promote a culture of acceptance. Promoting diverse narratives can serve as a powerful tool in fostering empathy, relieving misconceptions, and creating a more supportive environment for affected individuals.
Impact of Stigma on Prevention and Treatment
The stigma surrounding sexually transmitted infections (STIs) can have a profound impact on both prevention and treatment, acting as a significant barrier that deters individuals from seeking appropriate healthcare. Just as shadows obscure our vision, stigma clouds the realities of STIs, often leading to delayed diagnoses and increased transmission rates. When people carry the burden of stigma, they may avoid getting tested or treated for fear of judgment from healthcare providers or peers. This avoidance can perpetuate a cycle of silence and denial that affects larger public health efforts.
Research indicates that the internalization of stigma can lead individuals to experience shame and isolation, as they grapple with their STI diagnoses. This social disapproval can deter them from disclosing their status to partners or seeking necessary medical help. For example, a study from the CDC found that those who experience stigma surrounding STIs are less likely to communicate openly about their health with sexual partners. Without this dialogue, individuals remain unaware of their risks and continue to contribute to the cycle of transmission.
Furthermore, stigma discourages individuals from seeking regular screenings, often leaving STIs undetected until complications arise. Women, for example, are particularly vulnerable as asymptomatic STIs can have long-term effects, such as infertility or pelvic inflammatory disease. Like weeds in a garden, if left untreated, STIs can proliferate, causing a cascade of health issues that are more difficult and costly to manage compared to early intervention.
Strategies to mitigate stigma’s impact should include comprehensive public health campaigns emphasizing the commonality of STIs and the importance of regular testing. Additionally, integrating mental health support within STI treatment facilities can help individuals cope with feelings of shame and isolation, facilitating a more holistic approach to healthcare.
Ultimately, addressing the impact of stigma on prevention and treatment requires a multifaceted approach that combines public health education, supportive healthcare environments, and transparent communication about sexual health. By fostering open dialogues and dismantling harmful stereotypes, we can encourage individuals to prioritize their sexual health without fear.
The Science of Sexually Transmitted Infections
Understanding the science of sexually transmitted infections (STIs) is fundamental to effectively addressing their prevalence in society. Often, people perceive STIs as daunting and complex, similar to the intricate workings of a computer system. However, by breaking down their components and addressing their biology, transmission, and treatment, we can foster a better understanding and mitigate stigma.
Common Types of STIs Include:
- Chlamydia: This is the most prevalent bacterial STI, often asymptomatic in both genders. It can cause severe reproductive complications if left untreated.
- Gonorrhea: Known for its symptomatology including painful urination and discharge, gonorrhea’s widespread nature can lead to serious reproductive health issues if not addressed promptly.
- Syphilis: Unique in its progression through various stages, syphilis can lead to severe health consequences if diagnosed late. Each stage presents distinct symptoms and requires timely medical intervention.
- Human Papillomavirus (HPV): A viral infection that can result in genital warts and is linked to cervical cancer. Vaccines offer protection against the most harmful strains.
- Herpes Simplex Virus (HSV): Both HSV-1 and HSV-2 can cause painful sores. While there is no cure, antiviral medications can help manage symptoms and minimize outbreaks.
Key Points of Understanding STIs:
- Many STIs are asymptomatic, which means individuals might not know they are infected. This invisibility often leads to increased transmission rates since individuals are unaware of their status.
- The asymptomatic nature of many STIs demonstrates the need for regular screenings. Like routine check-ups for car maintenance, regular health checks can proactively address issues before they escalate.
- Effects on Health: STIs can significantly impact reproductive health and overall well-being, underscoring the importance of education and proactive healthcare efforts.
In essence, a greater understanding of STIs, including their types, transmission methods, and treatment essentials, enables individuals to approach their sexual health with informed confidence. Programs that integrate education about STIs into broader health curricula can revolutionize how we perceive and engage with sexual health, leading to reduced stigma and improved treatment outcomes.
Common Types of STIs and Their Effects
Sexually transmitted infections (STIs) encompass a wide range of pathogens that can profoundly affect the health of individuals and public health overall. The most common STIs can vary widely in symptomology, transmission methods, and long-term effects, highlighting the urgent need for education and understanding.
- Chlamydia:
- Effects: Often asymptomatic, chlamydia can lead to severe reproductive health issues such as pelvic inflammatory disease (PID) in women if left untreated.
- Symptoms: Pain during intercourse, abnormal discharge, and abdominal pain may occur but often go unnoticed, emphasizing the need for regular screening.
- Gonorrhea:
- Effects: Gonorrhea can lead to complications like infertility, especially in women. It may also increase susceptibility to HIV transmission.
- Symptoms: Painful urination and a pus-like discharge are common, but many may remain asymptomatic, perpetuating false security around one’s health status.
- Syphilis:
- Effects: Progresses through stages primary, secondary, latent, and tertiary each presenting diverse symptoms. Late-stage syphilis can lead to severe complications affecting the cardiovascular and nervous systems.
- Symptoms: Initial painless sores can go unnoticed, followed by rashes and systemic effects without treatment.
- Human Papillomavirus (HPV):
- Effects: Can lead to genital warts and is a major cause of cervical cancer. Vaccines are crucial for prevention but awareness remains low.
- Symptoms: Many infected individuals remain asymptomatic, causing HPV to spread silently.
- Herpes Simplex Virus (HSV):
- Effects: Though lifelong, symptoms can be managed through antiviral therapy. The stigma attached to herpes can significantly impact mental health and relationships.
- Symptoms: Painful sores during outbreaks are typically localized but can experience significant emotional distress and social stigma.
Transmission Methods and Risk Factors
Understanding how sexually transmitted infections (STIs) are transmitted is crucial in curbing their spread and reducing stigma. STIs are primarily spread through various sexual contact methods, including oral, anal, and vaginal intercourse. Here’s a breakdown of common transmission routes and associated risk factors:
Transmission Methods:
- Unprotected Sexual Contact:
- Most common method of transmission; includes all forms of sex (oral, anal, and vaginal).
- For instance, both gonorrhea and chlamydia can spread easily through unprotected intercourse.
- Mother-to-Child Transmission:
- Certain STIs like syphilis and HIV can be transmitted from an infected mother to her child during pregnancy, childbirth, or breastfeeding.
- This can result in significant health issues for infants, making prenatal care and testing vital.
- Infected Blood and Blood Products:
- HIV is a notable STI that can transmit through sharing needles or receiving contaminated blood transfusions.
Risk Factors:
- Multiple Sexual Partners: Having multiple partners increases the likelihood of exposure to STIs.
- Lack of Protective Measures: Avoiding condoms or protective barriers is a primary risk factor.
- Substance Abuse: Alcohol and drug use may impair judgement regarding safe sexual practices.
- Sexual Networks: Engaging in sexual networks where STIs are prevalent increases risk exposure.
Awareness of these transmission methods and risk factors is essential to foster safer sexual practices and mitigate the impact of STIs. Public health education initiatives can play a pivotal role in informing individuals about how to protect themselves and others, ultimately leading to healthier communities. The implementation of these initiatives should be culturally sensitive, addressing the unique needs and concerns within diverse populations.
Asymptomatic Infections and Their Challenges
Asymptomatic infections pose significant challenges in the management and treatment of sexually transmitted infections (STIs). Just as a silent storm can wreak havoc without warning, asymptomatic STIs can quietly proliferate, leading to severe health consequences for individuals and communities. Understanding the nature and challenges posed by asymptomatic infections is critical to recognizing their impact on public health.
Many STIs, such as chlamydia and gonorrhea, can remain undetected because they often do not exhibit noticeable symptoms. This invisibility contributes to the potential for continued transmission, as individuals may unknowingly infect their partners. The challenge lies in willing individuals to seek testing and treatment when they feel no immediate need to do so.
The implications of asymptomatic infections extend beyond individual health. Key challenges include:
- Delayed Treatment: Asymptomatic individuals may delay seeking care, resulting in untreated infections. For example, chlamydia can lead to PID in women if not identified and treated early, with potentially life-altering consequences.
- Continued Transmission: Without awareness or symptoms prompting action, asymptomatic individuals may unknowingly transmit infections to sexual partners, fueling the cycle of infection.
- Psychosocial Consequences: Upon eventual diagnosis, individuals might experience heightened anxiety and stress due to the stigma attached to STIs, especially if they perceive that they have unknowingly harmed others through transmission.
To effectively address these challenges, public health initiatives should emphasize routine screenings and education on the importance of testing regardless of symptom presentation. Campaigns could utilize creative strategies like interactive web and mobile applications that remind users of the importance of regular sexual health check-ups. In bringing awareness to the silent nature of many STIs, we can empower individuals to seek necessary care, ultimately reducing the prevalence of these infections in our communities.
The Importance of Education in Destigmatisation
Education plays a pivotal role in reducing stigma associated with sexually transmitted infections (STIs). By facilitating informed discussions and encouraging healthy behaviors, education can help cultivate understanding and empathy, akin to shedding light in a dimly lit room. Through comprehensive sexual health education, we can dismantle the prejudices and misconceptions that have fostered stigma historically.
- Awareness and Understanding: Accurate and accessible information about STIs, including modes of transmission and treatment options, can assuage fears and misconceptions. Like a well-lit pathway, clear information enables individuals to navigate their health choices confidently.
- Reducing Misconceptions: Many stigmas surrounding STIs stem from myths that can be dismantled through education. Understanding that STIs can affect anyone, regardless of their lifestyle, is essential for breaking down stigma and fostering a more compassionate societal approach.
- Fostering Empathy: Incorporating personal stories and testimonies about living with STIs can humanize these experiences, improving understanding and reducing judgment. This empathetic engagement is crucial in creating supportive environments for those affected.
- Encouraging Healthy Behaviors: Knowledge of STIs empowers individuals to take responsibility for their sexual health. Educational programs that emphasize safe practices can foster healthier approaches to sexual encounters.
- Community Engagement: Collaborating with local organizations and community leaders to deliver tailored educational initiatives fosters a collective understanding of STIs, enhancing outreach and reducing stigma.
- Policy Advocacy: Advocating for comprehensive sexual health education policies can underpin systemic changes necessary for dismantling stigma at broader levels. Informed individuals are better equipped to support health disparities and engage in constructive dialogues about sexual health.
In conclusion, education serves as the foundation for reducing stigma surrounding STIs, facilitating an environment where open dialogue and compassion flourish. By equipping individuals with knowledge and resources, we can empower communities to address sexual health more constructively, ultimately leading to improved public health outcomes.
Increasing Awareness About STIs
Raising awareness about sexually transmitted infections (STIs) is a critical component in the fight against stigma. Engaging in public health initiatives that foster understanding can help dismantle the stereotypes that have led to discrimination and misinformation surrounding STIs. Just as ripples spread outward from a pebble dropped in water, awareness campaigns can create a ripple effect that influences community norms and behaviors.
- National Campaigns: Public health organizations can leverage social media and traditional media to disseminate factual information about STIs. Campaigns that highlight common misconceptions and emphasize the importance of regular testing can foster community discussions.
- Conversations in Communities: Hosting community forums and workshops allows for open dialogues where individuals can discuss their concerns and experiences without judgment. Providing a safe space for these conversations encourages shared understanding and empathy.
- Storytelling as a Tool: Personal narratives from individuals living with STIs can humanize the issue, challenging harmful stereotypes and creating a sense of solidarity. These stories should emphasize the regularity and commonality of STIs, helping to normalize the experience.
- Educational Workshops in Schools: Providing accurate sexual health education in educational settings can significantly change perceptions about STIs among youth, instilling values of understanding and respect from a young age. Workshops can include interactive activities that promote knowledge and dispel myths.
Ultimately, increasing awareness around STIs requires a collective effort that involves various stakeholders, including health professionals, educators, and community leaders. By fostering conversations that prioritize knowledge, we can create an environment that reduces stigma and promotes health-seeking behaviors.
Comprehensive Sexual Education
Comprehensive sexual education (CSE) is a critical element of destigmatisation efforts regarding sexually transmitted infections (STIs). By providing young people with accurate information, CSE empowers them to make informed decisions about their sexual health and relationships. Much like a well-built foundation supports a house, well-structured sexual education lays the groundwork for healthy community dynamics.
- Curriculum Includes STIs: A robust CSE program should cover STIs, their transmission, prevention, and treatment in a factual, engaging manner. This information replaces misconceptions with knowledge, allowing students to understand the realities of STIs and their management.
- Promoting Healthy Relationships: Discussions around consent, communication, and respect form a vital part of CSE. By fostering these values, individuals can navigate relationships more confidently while reducing the risks associated with STIs.
- Addressing Cultural Sensitivities: CSE should take into account cultural differences and beliefs, ensuring inclusivity while promoting healthy sexual behaviors. By tailoring education to respect personal and community values, educators can effectively engage diverse populations.
- Empowering Young People: CSE instills a sense of agency, providing adolescents with the tools they need to make informed decisions about their sexual health. By ensuring that they understand their rights regarding consent and bodily autonomy, we can foster a generation that values respectful communications at all levels.
- Integration with Community Resources: Schools can partner with sexual health organizations to provide students access to additional resources and support, reinforcing the lessons learned in class.
In essence, comprehensive sexual education emerges as a cornerstone of destigmatisation efforts regarding STIs. By blending knowledge with empowerment and respect, CSE creates a supportive framework that enables individuals to make healthier choices, fostering positive relationships and healthier communities.
Myth-Busting: Facts vs. Fiction
Addressing misconceptions about sexually transmitted infections (STIs) requires a robust myth-busting approach. Misinformation can often act like an invisible barrier, preventing individuals from seeking help or discussing their sexual health openly. Just as correcting a false narrative can illuminate the truth, factual education can dismantle harmful myths surrounding STIs.
- Myth: STIs are a result of promiscuity.
- Fact: STIs can affect anyone, irrespective of their sexual history. They do not discriminate based on behavior but rather on exposure to the pathogens. Understanding this fact can help reduce the associated stigma and foster empathy for those affected.
- Myth: You can tell if someone has an STI by looking at them.
- Fact: Many STIs are asymptomatic, meaning individuals may not display visible signs or symptoms. Relying on appearance can lead to false security and increase the risk of transmission.
- Myth: All STIs are serious and life-threatening.
- Fact: While some STIs pose serious health risks if untreated, many, such as chlamydia and gonorrhea, are easily treatable with proper medication. Early diagnosis minimizes long-term complications.
- Myth: Using condoms guarantees 100% protection against STIs.
- Fact: While condoms significantly reduce the risk of STI transmission, they do not provide absolute protection. Some STIs can spread through skin-to-skin contact in areas not covered by the condom, mandating a comprehensive understanding of safe sexual practices.
By actively debunking myths and presenting factual information, health educators and advocates can empower individuals to engage in healthy sexual practices and seek care without fear. Developing engaging educational campaigns that emphasize the realities of STIs can reshape societal conversations and reduce stigma.
Psychological and Emotional Impact of STI Stigma
The psychological and emotional impact of stigma associated with sexually transmitted infections (STIs) can be profound, creating barriers to care and significantly affecting the quality of life for affected individuals. Just as a heavy weight can slow a person’s movement, stigma can hinder emotional and psychological well-being, making it essential to understand the consequences it poses.
- Psychological Distress and Anxiety: Individuals diagnosed with STIs often experience heightened levels of anxiety and depression due to internalized stigma and fears of judgment. Much like an unexpected storm can disrupt a calm day, the revelation of an STI diagnosis can severely impact an individual’s mental state.
- Fear of Disclosure: The fear of social repercussions can cause individuals to avoid disclosing their status to partners or close friends. This concealment can lead to feelings of shame, increasing one’s sense of isolation and exacerbating mental health issues.
- Impact on Relationships: STI stigma can complicate personal relationships, causing individuals to struggle with intimacy and trust. The fear of rejection may heighten feelings of unworthiness, adversely affecting their connections with others.
- Self-Esteem Challenges: The internalization of stigma can manifest as low self-esteem or reduced self-worth. Individuals may struggle to reconcile their identities with their health status, leading to negative self-perceptions that can hinder their emotional resilience.
- Syndemic Phenomenon: The relationship between STIs and mental health disorders can be defined as a ‘syndemic,’ where both manifest together, resulting in compounded adverse effects. This reciprocal dynamic suggests that addressing one component necessitates attention to the other for effective treatment and care.
Efforts aimed at destigmatizing STIs can substantially improve the mental health and well-being of affected individuals. Integrated approaches that foster open conversations about STIs, combined with supportive environments, can help mitigate the psychological impact of stigma. Creating community spaces that promote acceptance can empower individuals to seek care without fear, ultimately leading to healthier individual and community outcomes.
Mental Health Consequences
The intersections between mental health and sexually transmitted infections (STIs) are profound and multifaceted. In many ways, the challenges posed by STIs can exacerbate existing mental health conditions or trigger new psychological distress. Just as a tangled ball of yarn can create confusion, the intertwining effects of STIs and mental health can be challenging to unravel.
- Increased Risk of Anxiety and Depression: Individuals diagnosed with STIs may experience heightened levels of anxiety and depression, particularly in conjunction with the stigma associated with these conditions. Studies have indicated that mental health issues can intensify feelings of shame and isolation, creating a cycle that reinforces negative emotions.
- Social Withdrawal: Stigma can lead individuals to withdraw from social interactions and support networks, exacerbating feelings of loneliness. The resultant isolation can further fuel mental health challenges, as people may feel unsupported in managing their conditions.
- Internalization of Stigma: Internalized stigma can distort self-perception, making individuals feel unworthy or undeserving of love and care. This can lead to negative coping mechanisms and avoidance of healthcare services, resulting in worsening health outcomes.
- Impact on Relationships: Difficulty in disclosing STI status to partners can lead to strained relationships. Individuals may fear rejection, which can create emotional distance and hinder open communication, further complicating interpersonal dynamics.
- Importance of Support: Addressing mental health alongside STI treatment is crucial for holistic care. Integrated support systems that encompass mental health services can provide individuals with the tools to cope with the psychological ramifications of their diagnosis.
Promoting destigmatization is vital in enhancing mental health outcomes for those affected by STIs. By fostering open communication about sexual health and mental well-being, we can create greater understanding, resilience, and acceptance within communities.
Coping Strategies for Affected Individuals
Coping with the psychological and emotional impacts of sexually transmitted infection (STI) stigma requires effective strategies and supportive systems. Just like an athlete trains to build strength and resilience, individuals affected by STIs can adopt coping techniques to navigate the challenges they face.
- Seeking Professional Help: Engaging with mental health professionals who specialize in sexual health can provide invaluable support. These professionals can offer tailored coping mechanisms and therapeutic strategies to address the unique psychological challenges associated with an STI diagnosis.
- Building a Support System: Creating a network of understanding friends, family, or support groups can help diminish feelings of isolation. Support groups, whether in-person or online, allow individuals to share their experiences and challenges, fostering community and understanding.
- Educating Yourself: Knowledge about STIs including transmission methods and management options can empower individuals. Understanding one’s condition can help alleviate anxiety and foster a sense of control over their health.
- Practicing Self-Care: Prioritizing self-care routines, such as engaging in physical activities, maintaining a balanced diet, and practicing mindfulness, can enhance emotional well-being and reduce stress levels. Establishing a self-care routine can be akin to nurturing one’s mental garden, ensuring it thrives amidst challenges.
- Communicating Openly: Developing communication skills to discuss STI status with partners can strengthen relationships. Open discussions can promote understanding and reduce fears of judgment or rejection, ultimately leading to more supportive interactions.
Coping strategies and support systems are integral for those affected by STI stigma. By cultivating knowledge, building networks, and engaging in self-care, individuals can build resilience and reclaim their narratives with confidence.
Support Systems and Resources
Building effective support systems and accessing resources for individuals affected by sexually transmitted infections (STIs) is crucial for promoting well-being and reducing stigma. A comprehensive support system provides the comfort, knowledge, and empowerment required for affected individuals to navigate the complexities of their experiences.
- Healthcare Providers: Finding healthcare professionals experienced in providing sexual health support is vital. These providers must create a judgment-free environment that encourages confidential testing and open discussion about STIs.
- Support Groups and Organizations: Participation in support groups can connect individuals with peers who share similar experiences. Organizations like the American Sexual Health Association (ASHA) and the National Coalition of STD Directors (NCSD) offer resources, counseling, and forums for shared experiences.
- Advocacy and Educational Initiatives: Engaging with advocacy organizations can empower individuals by providing them with the tools to educate others about STIs. By participating in awareness campaigns, affected individuals can help destigmatize their health conditions.
- Online Resources: Many websites offer valuable information about STIs, including education on transmission methods, prevention, and treatment options. These platforms can serve as anonymous resources for individuals seeking guidance without the fear of being judged.
- Mental Health Support Services: Connecting with mental health professionals who understand the implications of living with STIs is vital. These specialists can provide coping strategies and support mechanisms tailored to the unique emotional landscape of affected individuals.
In essence, effective support systems and access to resources are paramount for individuals navigating the challenges associated with STIs. By fostering inclusive environments and encouraging open discussions, we can combat stigma and empower individuals to seek care, ensuring that they do not face the burden of their conditions in isolation.
Strategies for Destigmatising STIs
Destigmatisation of sexually transmitted infections (STIs) requires a concerted effort that includes enhancing public understanding, rewriting societal narratives, and fortifying community support systems. Like a comprehensive puzzle, effective strategies can help piece together a more cohesive and empathetic response to STIs.
- Community-Based Interventions: Implementing community-driven education initiatives can significantly reduce stigma surrounding STIs. Programs that involve local stakeholders and address specific community needs create a powerful platform for open discussions.
- Engaging Media Campaigns: Utilizing media campaigns that focus on real stories and encouraging dialogue around STIs can counteract negative stereotypes. Social media is a powerful tool for amplifying messages of acceptance and normalizing conversations surrounding sexual health.
- Public Health Education: Providing comprehensive sexual health education in schools and community centers can foster informed discussions about STIs. Ongoing education can diminish the divide between misconceptions and factual knowledge, counteracting stigma over time.
- Targeting High-Risk Populations: Engaging with specific communities disproportionately affected by STIs is essential. Tailored programs can address the unique challenges faced by these groups, fostering understanding and community support.
- Legislative Support: Advocating for policies that protect individuals with STIs against discrimination is critical. Ensuring equitable access to healthcare services and education can help create an environment where seeking care is prioritized over fear.
These strategies, when executed thoughtfully and inclusively, can contribute substantially to destigmatisation efforts. By reshaping societal narratives about STIs, promoting open dialogue, and fostering supportive communities, we can improve health outcomes and empower individuals to take control of their sexual health.
Community Interventions and Outreach Programs
Community interventions and outreach programs serve as vital arteries through which education, support, and stigma reduction can flow. Similar to a grassroots movement, these projects center on local engagement to enhance awareness and foster collective responsibility for sexual health. Successful community interventions can catalyze significant changes in how STIs are perceived and managed.
- Local Health Campaigns: Collaborating with local health organizations to run campaigns focused on STIs can significantly raise awareness. These initiatives can take various forms, such as health fairs, pop-up clinics, or workshops that deliver information in relatable, accessible ways.
- Peer Education Models: Training community members as peer educators creates an opportunity for genuine communication and trust-building. Peer educators can provide resources, share experiences, and inform their communities about the importance of testing and treatment.
- Support Networks: Developing peer-led support networks allows individuals living with STIs to connect, share insights, and provide emotional support to one another. These networks help mitigate isolation, challenge stigma, and promote a culture of open discussion.
- Engaging Local Influencers: Engaging respected community leaders and influencers to speak out about STIs can alter public perceptions. Their voices can help challenge stereotypes and provide a platform for nuanced discussions about sexual health.
- Utilizing Local Media: Leveraging local TV, radio stations, and newsletters for public health messaging can maximize reach and impact. Stories that illustrate real-life experiences can foster connection and empathy for those affected by STIs.
By prioritizing community engagement and outreach, we can create an inclusive environment where individuals feel supported in discussing and managing their sexual health. These programs promote a culture of understanding over shame, ultimately enhancing individual and public health outcomes.
Role of Healthcare Providers in Stigma Reduction
Healthcare providers play a crucial role in reducing stigma associated with sexually transmitted infections (STIs) through direct engagement with individuals seeking care. Just as a guide can illuminate a dark path, healthcare providers have the potential to navigate individuals through the complexities of STIs with empathy and understanding.
- Creating Non-Judgmental Environments: Training healthcare providers to communicate sensitively about STIs can foster a safe space for open discussions. Providers should prioritize non-judgmental language, actively engage in understanding patient experiences, and affirm their experiences, which can help dismantle stigma at the point of care.
- Promoting Routine Screening: Encouraging individuals to view regular STI screening as a standard health practice can normalize testing and reduce stigma. Providers can emphasize that STIs are common medical conditions, similar to other routine health checks.
- Education and Counseling: Providers should take the opportunity to educate patients about STIs, dispelling myths and misconceptions during appointments. Providing clear information about transmission and treatment options can empower patients while fostering a sense of agency over their health.
- Advocacy and Engagement: Healthcare providers can advocate for their patients beyond the clinical setting by engaging in public health initiatives that promote awareness and acceptance of STIs. Participating in community health fairs or educational workshops emphasizes their commitment to reducing stigma and improving sexual health.
- Collaborative Care Models: Integrating mental health assessments as part of STI treatment allows providers to address the psychological consequences associated with stigma. Offering comprehensive care that includes mental health support can enhance overall health outcomes for patients.
By actively engaging in stigma reduction efforts, healthcare providers can significantly impact individuals’ health-seeking behaviors and overall well-being. Their role as educators and advocates is pivotal in creating a supportive healthcare landscape that prioritizes understanding and compassion.
Engaging Media and Public Campaigns
Media and public campaigns are essential in reshaping perceptions surrounding sexually transmitted infections (STIs) and fostering an environment of acceptance and understanding. Just as a powerful narrative can captivate an audience, strategic campaigns can effectively challenge stigma and promote healthier attitudes towards sexual health.
- Storytelling Campaigns: Creating platforms for individuals to share their experiences living with STIs, whether through social media, videos, or articles, humanizes the issue and breaks down misconceptions. Personal narratives allow for connection and empathy, encouraging others to engage without fear of judgment.
- Celebrity Endorsements: Involving celebrities and public figures in STI awareness campaigns can leverage their influence to reach wider audiences. Their involvement can normalize discussions about STIs, prompting fans to re-evaluate their perceptions and attitudes.
- Social Media Engagement: Utilizing social media platforms for STI education fosters openness and allows for real-time discussions. Creative content, such as infographics, quizzes, and informative videos, can provide valuable information while engaging younger audiences.
- Community Challenges: Organizing public challenges or events promotes awareness and participation. For instance, a “STI Awareness Month” challenge can incentivize individuals to engage in testing, share resources, and advocate for education within their communities.
- Partnerships with Organizations: Collaborating with advocacy organizations can amplify campaign messages. Partnering with local health departments or NGOs can enhance access to resources and create a unified front in addressing STI stigma.
Engaging media and public campaigns must be strategic, inclusive, and empathetic to dismantle stigma and foster understanding effectively. By prioritizing transparency, education, and open dialogue, these initiatives can transform societal perceptions and encourage individuals to seek the care they need without fear.
Policy Changes and Public Health Initiatives
Policy changes and public health initiatives are vital components in the fight against sexually transmitted infections (STIs) and the stigma surrounding them. Just as legislation shapes societal norms, thoughtful public health policies can significantly improve health outcomes and foster environments conducive to education and acceptance.
- Supportive Legislation: Advocating for laws that protect the rights of individuals with STIs is essential in reducing stigma. Legislation should prioritize access to education, treatment, and preventive services while guaranteeing protections against discrimination.
- Integrated Health Services: Developing comprehensive public health strategies that incorporate STI prevention and treatment within primary healthcare frameworks can enhance access for all individuals. A unified approach can remove stigmas associated with seeking specialized STI care.
- Funding for Awareness Campaigns: Allocating resources for public health campaigns aimed at raising awareness about STIs is crucial. Funding should support initiatives that promote accurate information, reduce misconceptions, and foster open conversations around sexual health.
- Research and Evaluation: Ongoing assessment of public health initiatives and policies is vital for identifying effective strategies for STI prevention and stigma reduction. Research backed by data will enable responsive policymaking that meets the changing needs of communities.
- Collaboration with Community Organizations: Partnering with grassroots organizations can enhance outreach efforts by tailoring interventions to specific populations. Community-led initiatives can bridge gaps in services and address the unique challenges faced by underrepresented groups.
In conclusion, synergizing policy changes with public health initiatives creates an atmosphere where individuals feel supported in pursuing sexual health care. By integrating legislative support with community engagement, we can foster an informed population that prioritizes prevention and treatment, ultimately mitigating stigma and enhancing public health outcomes.
Importance of Supportive Legislation
The importance of supportive legislation in the context of sexually transmitted infections (STIs) cannot be overstated. Legislation plays a pivotal role in shaping public health policies that seek to reduce stigma and promote better health outcomes. Just as a sturdy framework supports a building, effective legislative measures provide the foundation for empowered individuals and communities.
- Protecting Rights: Supportive legislation should ensure that the rights of individuals living with STIs are upheld, providing protections against discrimination in healthcare settings and employment. This can foster an environment where individuals feel secure in disclosing their status and seeking care.
- Increased Access to Care: Legislative efforts can extend funding for STI testing, treatment, and education in underserved communities. By prioritizing access to care, such legislation can dismantle barriers faced by marginalized groups and reduce health disparities.
- Sexual Health Education Policies: Mandating comprehensive sexual health education in schools acts as a proactive measure for STI prevention. Education policies that emphasize knowledge and understanding empower individuals to make informed choices about their sexual health.
- Public Health Fund Allocation: Directing funds toward STI prevention programs, outreach efforts, and awareness campaigns is critical for effective public health initiatives. Legislative support can drive resource allocation to ensure communities can access essential services.
- Research Initiatives: Supportive legislation can prioritize research into the most effective methods of STI prevention and treatment. Evidence-based policies can facilitate the implementation of successful strategies to address STIs, supporting wider health initiatives.
Ultimately, supportive legislation serves as a cornerstone for addressing the issues surrounding STIs and deconstructing stigma. By empowering individuals through informed legal frameworks, society can break the cycle of shame and ignorance, leading to healthier communities.
Funding for STI Prevention and Treatment Programs
Funding for sexually transmitted infection (STI) prevention and treatment programs is essential in ensuring public health initiatives effectively address the growing concerns surrounding STIs. Just as a well-resourced garden produces vibrant blooms, consistent funding creates flourishing public health infrastructures that benefit communities.
- Global Health Initiatives: Significant investments are required to tackle STIs on an international scale. Organizations such as the World Health Organization (WHO) underscore the need for funding to develop comprehensive STI prevention strategies and bolster healthcare access worldwide.
- Locally Funded Programs: Community-based prevention and treatment initiatives require stable funding. Local health departments can coordinate resources toward initiatives that empower individuals with education, screening, and treatment options based on community needs.
- Emergency Funding for Health Disparities: In high-burden populations, targeted funding should address specific disparities impacting access to healthcare services. Allocating emergency resources towards vulnerable populations can effectively mitigate disease prevalence and improve overall public health.
- Evaluation and Accountability: Funding should include mechanisms for monitoring and evaluating program effectiveness. Investments must contribute to sustainable interventions that continuously adapt to community needs, improving health outcomes over time.
- Collaboration with Private Sectors: Collaborating with private organizations and non-profits can create diversified funding streams for STI prevention initiatives. Building partnerships can leverage resources and expertise for more effective health campaigns.
In conclusion, sustainable funding is a vital component of successful STI prevention and treatment programs. By ensuring that resources are allocated effectively, public health initiatives can flourish and adapt, paving the way for improved health outcomes and reduced stigma.
Global Perspectives on STI Management
Global perspectives on managing sexually transmitted infections (STIs) reveal both challenges and opportunities in addressing public health concerns. Just as a multifaceted diamond reflects light from numerous angles, effective approaches must incorporate diverse strategies tailored to unique cultural contexts, ensuring that all populations can access necessary care.
- Cultural Sensitivity: Approaches to STI management should be culturally informed, recognizing that attitudes towards sexual health vary across different communities. Adapting messages and programs to local customs enhances acceptance and engagement.
- International Collaboration: Efforts to combat STIs worldwide necessitate strong international partnerships that facilitate powerful knowledge-sharing and resource allocation. Organizations like UNAIDS foster collaboration, coordinating responses across borders to reduce stigmatization and improve access to care.
- Technology Advancements: The use of technology in STI management, such as telehealth services, allows for accessible testing and treatment options. Such innovations can bridge gaps in care, particularly in resource-limited settings, allowing individuals to receive support discreetly and efficiently.
- Public Health Policies: Countries with robust public health strategies often exhibit lower rates of STIs. Advocating for evidence-based policies including comprehensive sexual health education and accessible healthcare can effectively reduce incidence rates and destigmatize STIs.
- Research and Innovation: Global perspectives on STI research emphasize the importance of understanding emerging trends, epidemiology, and effective interventions. Investing in research capable of tracking changing patterns of STIs can inform better strategies for prevention and treatment.
Ultimately, global perspectives require a comprehensive understanding of the social, economic, and cultural factors influencing STI management. By engaging in collaborative efforts and responsive strategies, we can foster a more integrated approach to addressing STIs effectively.
Review of Evelin Dacker’s Perspectives
Dr. Evelin Dacker’s perspectives on destigmatising sexually transmitted infections (STIs) provide critical insights into how society can better understand and address the issue of STIs through open dialogues, education, and compassion. Her work emphasizes that the stigma surrounding STIs is deeply rooted in societal taboos about sexuality, leading to negative outcomes for individuals affected by these infections.
- STARS Framework: Dr. Dacker’s STARS framework Safety, Turn-ons, Avoids, Relationship Intentions, and STI Status serves as a valuable communication tool. This structure encourages individuals to engage in open discussions about their sexual health, promoting transparency and honesty in relationships.
- Sex-Positive Education: Emphasizing a sex-positive approach, Dr. Dacker advocates for comprehensive sexual education that celebrates sexual diversity and autonomy. Her philosophy aims to shift narratives around STIs from shame to empowerment, promoting informed choices.
- Holistic Perspectives: Integrating discussions around mental health with sexual health, Dr. Dacker highlights the importance of emotional well-being in managing STIs. This holistic viewpoint fosters a deeper understanding of how stigma can affect overall health outcomes.
- Community Engagement: Dr. Dacker emphasizes the significance of community involvement in outreach programs. By fostering dialogue within communities, her approaches aim to normalize conversations around sexual health, facilitating greater understanding and acceptance.
- Advocacy for Policy Change: Dr. Dacker calls for systemic changes that prioritize equitable access to healthcare. Her advocacy for comprehensive sexual health policies underlines the need for legislative action to protect the rights of those affected by STIs.
Dr. Evelin Dacker’s perspectives provide a rich tapestry of insights that illuminate the necessary pathways toward destigmatization. By prioritizing education, communication, and advocacy, her work lays the groundwork for a more accepting and informed society.
Key Arguments and Recommendations
Dr. Evelin Dacker’s work encompasses compelling arguments and recommendations aimed at destigmatising sexually transmitted infections (STIs) through education, community engagement, and supportive legislation. Her multifaceted approach underscores the need for a paradigm shift in societal perceptions of STIs:
- Destigmatization through Education: Dr. Dacker champions comprehensive sexual education that encompasses diverse experiences and identities. Her recommendations stress the importance of removing misinformation and ensuring accurate information about STIs reaches all demographics.
- Engagement with Affected Populations: Acknowledging the lived experiences of individuals affected by STIs is crucial for creating inclusive dialogue. Dr. Dacker advocates for programs that elevate voices from marginalized communities, ensuring their needs and concerns are addressed.
- Promotion of Open Communication: Encouraging open conversations about sexual health, particularly surrounding sexual histories, enhances understanding and empathy. Dr. Dacker’s STARS framework serves as a practical tool to facilitate these discussions in both personal and clinical settings.
- Supportive Policies and Practices: Dr. Dacker calls for policy changes that support individuals with STIs, ensuring protections against discrimination in healthcare, employment, and society. Legislative advocacy for equitable access to care is paramount for effective intervention.
- Integration of Mental Health Services: Recognizing the psychological impact of STI stigma, Dr. Dacker recommends integrating mental health support within sexual health services. Providing comprehensive care that addresses both physical and mental health can lead to improved outcomes for affected individuals.
These key arguments and recommendations serve as essential cornerstones for a progressive approach to addressing STIs. By fostering an environment of education, open dialogue, and compassionate care, we can create a more supportive framework for individuals and communities grappling with the stigma of STIs.
Critical Insights from the Book
Dr. Evelin Dacker’s work provides critical insights into the complexities surrounding sexually transmitted infections (STIs), illuminating the stigma that often accompanies them and emphasizing the necessity of a comprehensive, informed approach. The following insights encapsulate her contributions:
- Understanding the Cultural Context: Dr. Dacker emphasizes the importance of examining the cultural narratives that shape perceptions of STIs. Understanding how societal beliefs influence attitudes can inform effective public health strategies.
- Destigmatization through Dialogue: Open conversations about STIs are essential for dismantling stigma. Dr. Dacker advocates for environments that foster dialogue between partners, friends, and healthcare providers, enabling individuals to discuss their sexual health freely.
- The Role of Personal Narratives: Highlighting the power of personal stories, Dr. Dacker illustrates how sharing experiences can challenge societal norms and facilitate understanding and empathy toward individuals affected by STIs.
- Empowerment through Knowledge: Dr. Dacker underscores the significance of education in advancing a sex-positive culture. Equipping individuals with accurate knowledge empowers them to make informed decisions and reduces stigma surrounding STIs.
- Interconnection of Health and Well-Being: Central to Dr. Dacker’s insights is the understanding that sexual health is interconnected with mental health. Addressing psychological needs alongside physical health is essential for comprehensive care.
In conclusion, Dr. Evelin Dacker’s work offers profound insights that contribute to the ongoing discourse surrounding STIs and their impact on individuals and communities. By prioritizing education, dialogue, and a nuanced understanding of sexual health, we can pave the way for a more compassionate, informed society.
Practical Applications of Dacker’s Work
Dr. Evelin Dacker’s work provides practical applications that individuals, healthcare professionals, and communities can employ to destigmatise sexually transmitted infections (STIs) and foster an environment of support and understanding. Through these applications, we can bridge the gap between knowledge and practice, creating lasting change in public health attitudes and behaviors.
- Implementation of the STARS Framework: Utilizing the STARS framework (Safety, Turn-ons, Avoids, Relationship Intentions, and STI Status) in personal and clinical conversations enables individuals to engage openly about their sexual health without fear of judgment. This framework cultivates transparency and reinforces healthy communication in relationships.
- Conduction of Community Workshops: Organizing workshops focused on sexual health education can provide valuable information and resources to communities. These sessions can incorporate peer-led discussions that address stigma, encourage testing, and highlight local resources.
- Integration of STI Education in Schools: Advocating for comprehensive sexual education in schools ensures that young people receive vital information about STIs before entering sexually active adulthood. By providing accurate knowledge at an early age, we can establish a foundation of understanding and acceptance.
- Collaboration with Health Professionals: Training healthcare providers to apply Dr. Dacker’s insights into practice not only equips them to address stigma but also enhances patient care. Providers who utilize inclusive language and approaches are more likely to encourage open discussions about sexual health.
- Engagement in Social Activism: Advocating for policy changes that protect individuals living with STIs can help create supportive frameworks. By participating in awareness campaigns and local activism, individuals can contribute to a larger movement that seeks to dismantle stigma regarding STIs.
In sum, the practical applications of Dr. Dacker’s work offer various pathways for individuals and communities to advance the destigmatisation of STIs effectively. By employing these strategies, we can foster environments of understanding, empowerment, and optimal sexual health.
Conclusion on Destigmatisation Efforts
Destigmatising sexually transmitted infections (STIs) is an essential endeavor that requires a multifaceted approach involving education, community engagement, and systemic changes within healthcare and public health policies. By recognizing the importance of understanding stigma, promoting compassion, and fostering open discussions about sexual health, we can pave the way towards a healthier society that encourages individuals to seek care without fear. Dr. Evelin Dacker’s work serves as a guiding light, illuminating pathways toward destigmatisation through practical strategies that enhance communication, empower individuals, and promote informed care. Together, we can break down barriers, dismantle harmful narratives, and create a supportive environment for all individuals affected by STIs.
Future Directions in STI Education and Awareness
The future of STI education and awareness lies in creating innovative, inclusive, and dynamic strategies that expand understanding while reducing stigma. Like a thriving ecosystem, this approach necessitates collaboration, continuous learning, and adaptability.
- Leveraging Digital Platforms: Increasing the use of digital platforms in education and outreach can enhance engagement, especially among younger populations. Interactive apps, online courses, and social media campaigns can facilitate access to accurate information.
- Emphasizing Intersectionality: Future educational initiatives should address the intersectionality of STIs with various social determinants of health. Understanding how factors like race, gender identity, and socio-economic status influence STI experiences can foster connection and inclusivity.
- Encouraging Peer-to-Peer Support: Creating peer-led support networks can foster community resilience and improve mental health outcomes. Peer advocates can provide relatable experiences, share insights, and normalize discussions surrounding STIs.
- Sustained Public Health Initiatives: Continued investment in public health initiatives that prioritize STI education, testing, and treatment will be essential to maintaining progress. Collaboration among healthcare providers, educators, and community organizations can contribute significantly to combating stigma.
- Global Knowledge Exchange: Engaging in global dialogues about STI prevention strategies can enhance local approaches. Sharing best practices across international lines can inspire innovative solutions tailored to unique cultural contexts.
By embracing these future directions, we can foster a paradigm shift in societal attitudes toward STIs, effectively destigmatising these infections and empowering individuals to take control of their sexual health narratives. Together, we can advocate for a brighter, more informed future in the realm of sexual health.
Frequently Asked Questions:
Business Model Innovation: We use a group buying approach that enables users to split expenses and get discounted access to well-liked courses.
Despite worries regarding distribution strategies from content creators, this strategy helps people with low incomes.
Legal Aspects to Take into Account: Our operations’ legality entails several intricate considerations.
There are no explicit resale restrictions mentioned at the time of purchase, even though we do not have the course developers’ express consent to redistribute their content.
This uncertainty gives us the chance to offer reasonably priced instructional materials.
Quality Assurance: We guarantee that every course resource you buy is exactly the same as what the authors themselves are offering.
It’s crucial to realize, nevertheless, that we are not authorized suppliers. Therefore, the following are not included in our offerings:
– Live coaching sessions or calls with the course author.
– Entry to groups or portals that are only available to authors.
– Participation in closed forums.
– Straightforward email assistance from the writer or their group.
Our goal is to lower the barrier to education by providing these courses on our own, without the official channels’ premium services. We value your comprehension of our distinct methodology.
Be the first to review “Destigmatising STIs: Understand Sexually Transmitted Infections By Evelin Dacker” Cancel reply
You must be logged in to post a review.


















Reviews
There are no reviews yet.